29 September 2022
Cancer immunotherapies assist the body’s immune system to hunt and kill cancerous cells with cell-by-cell precision.
By comparison, surgery, radiotherapy, and chemotherapy inflict significant collateral damage.
The analogy would be to compare carpet bombing to precision guided munitions.
The stakes are high in the search for a new breed of cancer cures with the global oncology market worth a reported USD$141.33 billion and expected to grow to USD$394.24 billion by 2027.
A guide to understanding immunotherapy. In this article...
- What is cancer?
- Traditional cancer treatment - cut, burn, poison
- Immunotherapy: the new frontier of cancer treatment
- Immune system challenges - how cancers evade detection
- Immunotherapy - assisting the immune system to identify cancer
- Immunotherapy treatment strategies
- Other immunotherapy challenges
- Australian biotech companies working on immunotherapies
- Cancer research in Australia
What is cancer?

The simple explanation is that cancer is abnormal growth arising from normal cells becoming mutant.
Mutation is not only natural but essential for evolution. Mutation occurs when cells replicate but don't faithfully duplicate their DNA - an error occurs. While such mutation is essential for species adaption, within the body mutation can lead to cancers.
Mutation results in a faulty new cell. Mutations happen all the time in the human body.
On average, the human body produces eight cancer cells per day.
Natural cancer protection systems
Sometimes a mutated cell is so faulty - the cell dies. Problem solved.
However, depending how the dice fall, some mutated cells still function, but it isn't always bad, there are mechanisms that automatically recognize and destroy abnormal cells. Normally faulty cells have a self-regulation function (part of the cell's apoptosis mechanism) that will release proteins (caspases) that destroy the cell from within. The cell suicides. Body functions then mop-up the remains of the dead cell.
Faulty cells also have the ability to self-repair some DNA faults.
Failing self-repair or suicide, the body's immune system is on the look-out for erroneous cells and destroys them.
So, the body has many natural defences to deal with random cell mutation.
And with billions of cells throughout the body continually dying and being replaced this process is continuous and normal.
Cancer is a game of chance
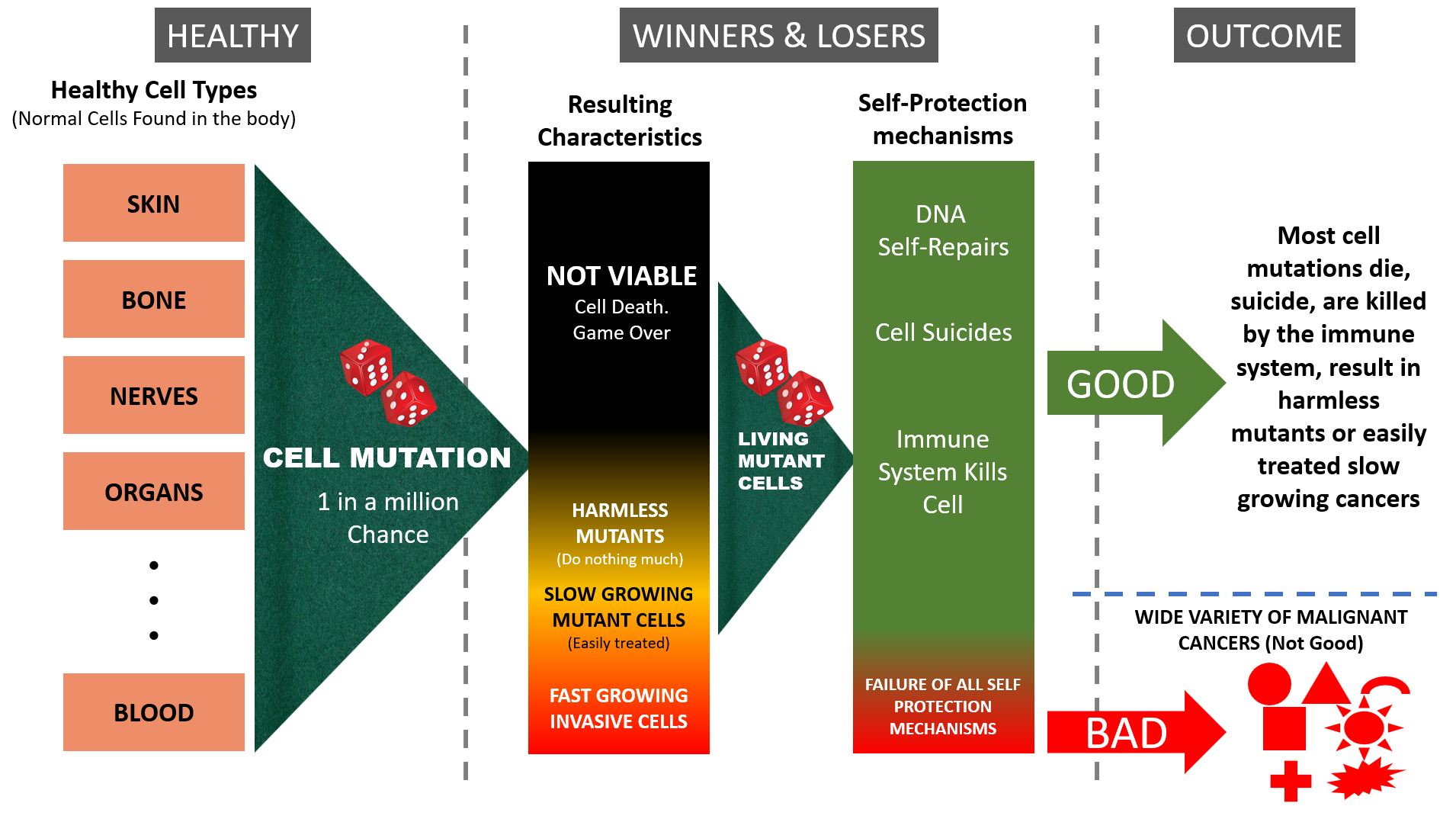
However, despite all of the above mechanisms that prevent mutated cells from having a future, sometimes mutant cells win the lottery and have the right set of characteristics to become problematic...
- Accumulated genetic mutations: Mutation often doesn't result in cancer. As normal cells replicate minor genetic variations can occur without triggering immune response, cell- suicide, or other protection mechanisms. But these genetic mutations will accumulate over time setting-up the precedence for the final mutation that may turn cancerous. This explains why the likelihood of developing cancer increases with age. So, while cancer is a game of chance, the odds get worse (as in, cancer is more likely) as we age.
- Have the required ability to sustain themselves and in some cases with increased vigor.
- Survive because their normal cell death and replication limiting mechanism (apoptosis) is also faulty due to mutation (or accumulated mutations).
- The body's immune system fails to recognize the damaged cells as abnormal. Either because the immune system is compromised or because the mutated cells lack characteristics that the immune system uses to recognize them as abnormal, or has acquired features that act as a cloaking mechanism that prevents identification.
- Fail to heed growth limitation signals: normal cells communicate with each other and are differentiated to ensure they form useful body parts (organs, ears, noses, skin, glands etc.). Abnormal cells are said to be undifferentiated - and just keep growing willy-nilly.
- Grow voraciously, crushing healthy surrounding structures compromising their normal function as the mutant cells replicate and occupy more space.
- Rob the body's resources to feed their growth (often the first sign of cancer is unexplained weight loss)
- Create life threatening bio-chemical imbalances. Curiously, cancer cells tend to switch from mostly aerobic to mostly anaerobic energy production generating more lactic acid (The Warburg Effect). Anaerobic energy production is inherently inefficient burning glucose at a greater rate. In addition, some cancer cells generate metabolites that are toxic.
- Grow with such aggressiveness the body can't feed all of the abnormal cells in a cancerous mass (hypoxia and glucose deprivation due to inadequate angiogenesis). The cancerous mass then consists of both rapidly growing cancer cells and cancer cells that have died (a nasty mess). The resulting necrotic (dead) tissue (tumor necrosis) poisons the body through massive infection and inflammation.
- Metastasize: aggressively growing cells are prone to breaking into blood vessels or lymphatic vessels and traveling to other parts of the body. Eventually they lodge somewhere and start a new colony.
- Tumour heterogeneity: Another tricky thing about aggressively growing cancers is their propensity to further mutate. Thus, the oncologist may specify a chemotherapy that has initial success shrinking a tumor only later to find the tumor starts to accelerate in size. The tumor is no longer exactly the same tumor; parts of it have mutated and developed a chemo resistant strain that then takes over the fight. This is one of the main reasons why chemotherapy is rarely a cure and more a death delaying tactic.
This chaotic situation is simply referred to as cancer but, this overly simplistic term hides the complexity of the disease.
Cancers vary widely in their aggressiveness, propensity to Metastasize, and other characteristics. Not all are life threatening.
Now, the astute reader will see the puzzle immediately.
Is this an immune system defect, a purely chance event, a problem with inherited DNA, or the result of an external agent or poison?
And the fact that the same types of cancers occur in different people suggests there is some pattern to this randomness.
More perplexing is why is it that 2 out of 3 people never develop cancer?
Including the majority of heavy smokers (but, cancer isn't their only risk).
The answer is, it is all of the above. The combinations of contributing factors are huge, and the outcomes create many different types of cancer that require differing treatments. Because cell mutation is random and produces unique new cells cancer is complex which doesn't help the potential development of universal prevention, treatment, or cure.
Traditional cancer treatment - cut, burn, poison

There are three ways to treat cancer...
- Surgery: cut the cancer out hoping that the cancer hasn't metastasized. Surgeon's aim to capture all of the cancerous mass, while being careful to limit damage to surrounding tissue and normal structures. Surgeons have to be careful to excise all of the cancer and even be careful not to have cells drop-off the mass as they are removing it falling back into the wound. Any remaining cells can start a new colony. Which is often the reason why surgery is followed-up with other treatments.
- Bombard it with radiation: kill the cancerous tissue with ionizing radiation with sufficient precision to limit damage to surrounding healthy tissue.
- Chemotherapy: find a chemical that is more poisonous to the cancerous cells than it is to healthy cells. Increasing the dosage to a threshold that kills the cancer but is just short of killing the person. More sophisticated chemotherapy agents can target specific cancer cells exploiting biochemical or cell functions that are peculiar to that type of cancer thereby reducing or avoiding damage to normal cells. This more targeted option is limited to certain types of cancers.
Oncologists determine the type of cancer and the nature of the disease progression in an individual and tailor a treatment plan (using one or a combination of the above tools) aimed at maximizing the patient's survival.
Years of research and clinical practice have refined these techniques to a high level of sophistication, specificity, and effectiveness but still people die from cancer.
Now medical science is exploring a new tool to add to the kit; helping the body to kill cancers by tuning the body's own immune system to attack and eradicate the cancer.
Immunotherapy: the new frontier of cancer treatment
The traditional cancer treatments listed above are ham-fisted compared with the body's own immune system which (when it works) has the ability to accurately select cancer cells for destruction with cell-by-cell precision. Traditional treatments (the three listed above) inflict significant collateral damage.
The analogy would be to compare carpet bombing to precision guided munitions.
Immunotherapy or immuno-oncology is recognised as the leading development in cancer treatment globally.
It is seen as a radically different approach to traditional chemotherapy and radiotherapy and represents a new frontier in the cancer battle.
Immune system challenges - how cancers evade detection
The immune system is a complex network of cells and organs that constantly fights disease, illness and infection.
The principal challenge is that the immune system is geared to detect and fight viruses, fungi, parasites, and bacteria (antigens) but cancer cells are not antigens they are mutated versions of the body's own cells.
As explained above, mutation in living tissue is common and normally mutated cells either aren't compatible with life and die naturally, self destruct, or mark themselves as defective allowing the immune system to do its job. Mutated cells are routinely removed as part of normal life.
Cancer is the rare situation where the mutation develops protection mechanisms through plain rotten bad luck (after all, mutation outcomes are highly random) and the cells are not only robust but also invisible to the immune system.
And while many people have trouble understanding how it is purely by chance that random mutation can result in a damaged cell that not only lives but also has the requisite mechanisms to evade the immune system and grow aggressively, consider that there are billions of cell reproductions taking place. There are many shots at goal.
However, due to the randomness of mutation there are also myriad ways through which cancer evades the immune system.
Immunotherapy - assisting the immune system to identify cancer
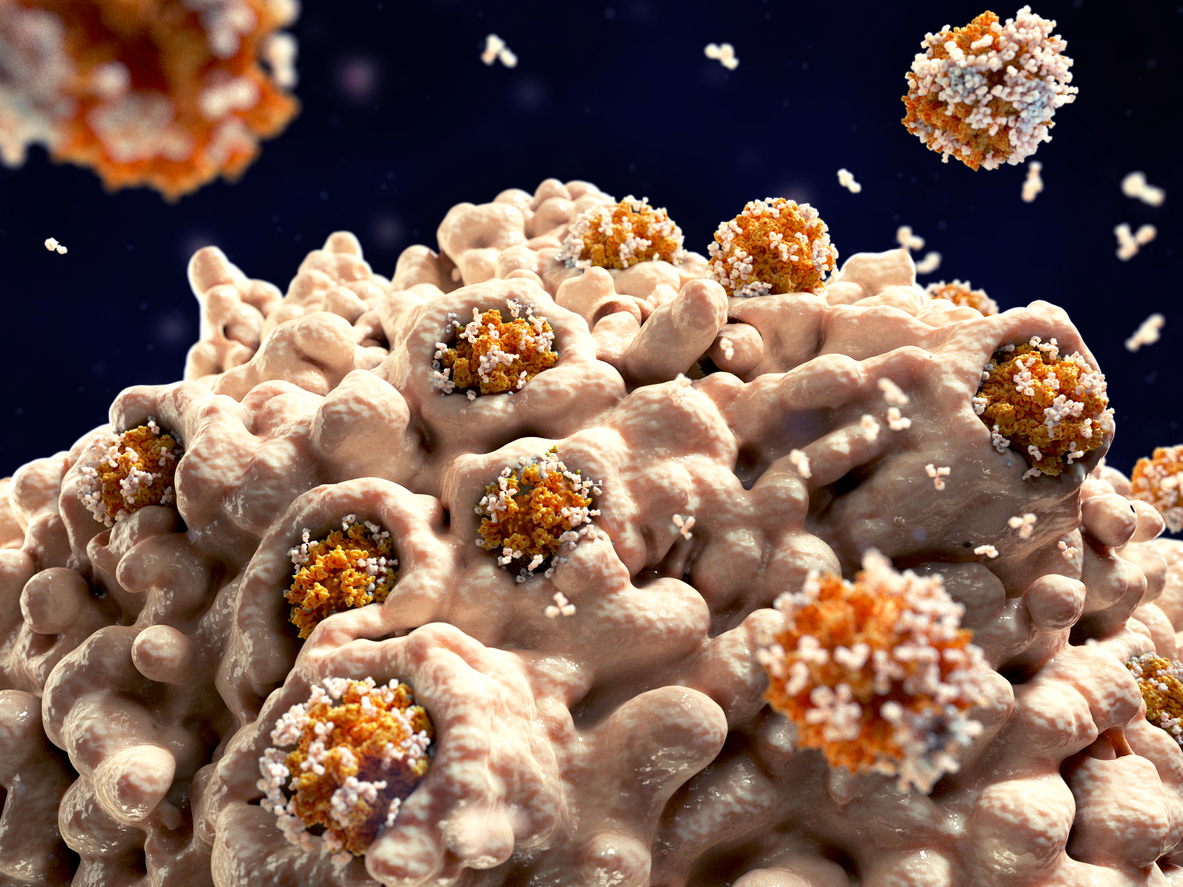
Put simply, immunotherapies work to assist the body’s own natural immune response to identify and combat cancerous cells.
The general approach is to identify a feature unique to cancer cells that distinguishes them from normal cells that can be exploited to assist the immune system to target and destroy the cancer cells.

In an ideal world there would be ONE distinguishing feature of ALL cancer cells that was both universal, easy to exploit, and the exploit treatment was safe to use. And immunotherapy researchers are working toward this goal.
For example it is known that cancer cells have abnormal gene structures, grow and divide at an abnormally rapid rate, are poorly differentiated, have abnormal cell membranes, cytoskeletal proteins and morphology, and produce energy mainly using anaerobic mechanisms associated with increased glycolysis as a result of upregulation of several major glycolytic enzymes.
Cancer cells suppress and deactivate genes and pathways that normally enable cells to die. Cancer cells become self-sufficient in producing growth signals (pathological mitosis) through the activation of oncogenes, and become insensitive to growth-inhibitory (antigrowth) signals. Cancer cells acquire the capacity to draw out their own supply of blood and blood vessels (tumor angiogenesis).
There are many other characteristics that cancer cells have that normal cells don't.
Researchers are even exploring differences at a molecular level in an effort to find an exploitable distinguishing feature
All of these represent an opportunity to select cancer cells using viral, biochemical, synthetic proteins, or some other process. The trick is finding something that works without inflicting further damage.
Cancer research is extremely challenging. Theories have to be carefully investigated and laboratory tested often for years before they show promise or can even be ruled out.
Failing developing a single universal approach, it may be possible to develop several universal treatments specific to the original cell types.
Cancers can be segmented as carcinomas (derived from epithelial cells), sarcomas (derived from bone and soft tissues), leukemia (from the blood forming tissue of the bone marrow), lymphoma (derived from lymphocytes), mutliple myeloma (cancer derived from plasma cells), melanoma (derived from skin pigment cells), brain and spinal cord tumors, germ cell tumors (derived from reproductive system cells), neuroendocrine tumors (derived from hormone producing cells), and carcinoid tumors (typically endocrine cells in the gut). And there are sub-segments.
Cancers deriving from mutation of each of these cell types have commonalities that may be exploited to develop targeted immunotherapies.
In addition, cancer cells can be traced back to the body part cells that they mutated from (lung tissue, breast tissue, bowel tissue etc.)
However, currently most Immunotherapy treatments being developed are less universal and more specific and a 'broad spectrum' approach remains elusive.
Immunotherapy treatment strategies

Typical immunotherapy treatment strategies are...
- Some cancers are only partially protected from the immune system. Artificially boosting the immune system can tip the balance toward defeating the cancer.
- Artificially mark the cancer cells so the immune system identifies them as antigens.
- Modify the body's own immune system cells to recognize cancer.
- Introduce modified viruses that are tuned to recognize and kill cancerous cells (and ignore healthy cells).
- Defeat the masks that some cancers exhibit that enable them to hide from the immune system.
- Teach the immune system to fight the cancer cells (exploiting the immune system's own adaption mechanism).
Each of those approaches is highly dependent on the type of cancer being treated and on the natural variations between each person's immune system.
Immunotherapies are categorized as...
-
Monoclonal Antibodies: MABs are artificially produced anti-bodies designed to bind to the surface of a cancer cell thereby marking it as a cell for the immune system to attack. MAB therapies mimic natural antibodies but are made in a laboratory.
-
Immune Checkpoint Inhibitors: The immune system is regulated by specific proteins that turn on or off an immune response. These are called checkpoint proteins and their usual function is to limit the activity of T-cells so they don't start attacking healthy cells. Some cancer cells release high levels of proteins that inhibit T-cells. Immune Checkpoint Inhibitors control these proteins to enable the immune system to attack the cancer cells. Two prominent checkpoint inhibitor therapies currently in-market are Pembrolizumab (Keytruda) and Nivolumab (Opdivo) which are effective in about 25% of patients that have cancers that are known to respond to these treatments.
-
Adoptive Cell Therapies: is another strategy to modify the immune system to recognize tumor cells. The method is to take cells (either cancer cells or immune cells) from the patient's body, modify them in the lab to enhance a positive effect on the immune system, and then reintroduce them to the body. There are three general approaches to ACT; 1) tumor-infiltrating lymphocytes (TIL), 2) ACT using T cell receptor (TCR) gene therapy, and 3) ACT with chimeric antigen receptor (CAR) modified T cells. Currently, there are up to six different CAR-T therapies approved by the FDA (US Federal Drug Administration) for use in the United States: Kymriah (Novartis), Yescarta & Tecartus (Kite), Breyanzi & Abecma (Bristol Myers Squibb), and Carvykti (Legend Biotech).
-
Oncolytic Virus Therapy: The inspiration for Oncolytic Virus Therapy was noticing that some cancer patients went into remission after contracting a viral infection. Further, it has long been observed that the Hepatitis virus selectively infect only liver cells. There are other examples where viruses are selective to particular cells. An Oncolytic Virus is a virus that tends to infect and kill cancer cells. Thus research has been developing cancer killing viruses. These viruses are found in nature as well as viruses modified in the laboratory. Researchers are hopeful that some oncolytic viruses may also trigger an immune response against the cancer. The initial virus attack on the cancer cells brings about cell death and releases materials (cell lysis) that may then be recognized by the immune system as foreign. This trains the immune system to recognize cancer cells and takeover from the virus to eradicate the cancer. Genetically modifying any virus has risks. The trick is to find a virus that so modified remains stable and doesn't itself mutate into something unexpected. Australian Imugene (ASX:IMU) is currently trialing its CF33 Virus Therapy independently and in combination with checkpoint inhibitor Pembrolizumab. Early results are showing that CF33 may have the remarkable ability to kill not just one type of solid tumor but ALL solid tumors (Professor Yuman Fong - City of Hope Medical Centre).
-
Cancer Vaccines: cancer vaccines are not yet a prevention but a cure. The approach is to give the patient a vaccine with similar antigen properties as the cancer but in a more easy to detect form. This encourages the immune system to develop anti-bodies that are able to more readily recognize and attack the cancer. Conventional vaccination is achieved by introducing a harmless form of the antigen so that the immune system can set-up specific defences. Cancer vaccination works in a similar way by either taking cancer cells from the patient and modifying them so they are more easily recognized or modifying a naturally occurring pathogen to mimic biochemical properties of the target cancer.
-
Immune System Modulators: delivering tailored immune cells to supplement an immune response. Sometimes the body's immune system is overwhelmed by the cancer and can't kill the cancer faster than it is growing. Immune System Modulators either enhance the performance of the entire immune system or specific components of it (white blood cells, T-cells, or antibodies for example) to boost immune system capacity.
-
Hybrid therapies: researchers are also experimenting with immunotherapies that combine one or more of the above approaches and/or with conventional chemotherapy (so-called "combo treatments"). Australian Imugene (ASX:IMU) is experimenting with combining immunotherapies. Imugene has one approach that first uses onCARlytics to designate cancer cells with CD19 protein and then using cell therapy to attack the cancer cells. Tumor cell lysis leads to viral particle release promoting an endogenous immune cell response.
Initial data suggests highly positive results potential, although it is important to note that it won’t work for everyone, and that (at the moment) immunotherapies are not suitable (or available) for the treatment of all types of cancer.
But, mostly the problem is that Immunotherapy science is a work in progress. Cancer is a giant jigsaw puzzle and scientist are working hard to assemble the pieces to form a complete immunotherapy picture.
Other immunotherapy challenges
There are numerous other challenges. Fast growing cancer cells have a propensity to further mutate just as their ancestor did. Purely through the power of chance, they develop new slightly different cells. The unique cell characteristics that scientists relied on to attack the original cancer cells (through developing innovative immunotherapies) may no longer be present.
Just as mutation is the basis for species adaption and survival, the same applies to cancer cells. Immuno-oncolgists resort to combination therapies to combat this.
Significant research is underway to develop immunotherapies into main stream treatments with greater cancer treating potency with less deleterious affects on the body.
A Deloitte Access Economics Report (2017) found that fewer than 2% of Australian cancer patients have access to immunotherapies, with recognised impediments of awareness, availability, and affordability.
Immunotherapies have foreseen a shift in research focus to a molecular level. It has seen a move from a traditional R&D focus on cancer defined by body part – breast, ovarian, pancreatic, prostate etc. to focusing on the molecular characteristics of tumors. A broader approach hopes to break-away from what has been a siloed approach to cancer research and development. [Deloitte et al.].
It's very early days, but developing less specific cancer treatments and a smaller set of more universal (broad-spectrum) treatments is the Holy Grail.
Australian biotech companies working on immunotherapies
Several ASX listed biotech companies are on the journey to commercialise therapies, offering hope to pancreatic, brain, gastric and ovarian cancer sufferers, and more.
These include...
- A spin-out company from the CRC Amplia Therapeutics Ltd (ASX:ATX)
- Chimeric Therapeutics Ltd (ASX:CHM)
- Noxopharm Ltd (ASX:NOX)
- Imugene Ltd (ASX:IMU)
- Kazia Therapeutics Ltd (ASX:KZA)
- Race Oncology Ltd (ASX:RAC)
- Arovella Therapeutics Ltd (ASX:ALA)
- and others.
The hope is that these Australian companies (and their overseas counterparts) will develop a whole new range of treatments for cancer offering greater precision and effectiveness with less harmful side effects.
Cancer research in Australia

Australia is seen as a leader generally in cancer medical research with an established and highly regarded research eco-system, however, we have not been so good at translating research breakthroughs to commercial opportunity.
Difficulty raising capital is one of the reasons that Australian companies exit or sell to big pharma companies, as the investment required to bring research from pre-clinical to clinical trial can run to the 100s of millions of dollars.
Over the last 8-10 years, Australia has worked to address weaknesses in the commercialisation of immunotherapies as it strives to move further up the chain in the high value pharma market.
The Cancer Therapeutics CRC was established in 2007 to plug this gap with a focus on leveraging Australia’s strong immunology capability across Australia.
In the course of operation, the CRC commercialised multiple drug discovery projects, secured over $40 million in licensing revenue, overseeing commercial partnering deals with Merck and Pfizer (2 of the largest preclinical deals in Australia). The CRC successfully transitioned to a private company (Canthera Discovery) in December 2020.
According to the World Health Organization (WHO), cancer is the second leading cause of death globally. In Australia in 2018 (last recorded data), the total number of cancer deaths was 49,500.
Research by the Cancer Council NSW has revealed the cost of cancer to the Australian health system to be over $6 billion a year and rising, with an ageing and increasing population.
Cancer is big business. It is also a tragic and often painful killer. One third of us develop some form of cancer in our lifetime. The quest for more effective detection and treatment is relentless.
It’s a slow race to a common end goal – to help cure cancer.
Further Information
- Interview with Brett Carter CEO of Cancer Therapeutics CRC
- Deloitte Access Economics – The New Wave of Immunotherapy Cancer Treatments – The Untapped Potential for Australians
- The draft Australian Cancer Plan will be released for public consultation later this year
- Estimating the cost of cancer to Australia’s health service – Cancer Council NSW
- Why do the majority of people never get cancer?
- Synthetic proteins [Scientific American].
- The biology of cancer [Boston University School of Public Health]
- Imugene Investor Presentation | non-deal road show August 2023
