19 December 2019
The heartwarming story of Australian genius Dr Daniel Timms and his journey developing the world's most advanced artificial heart.
An updated version of the original article published on this Blog in March 2015.
Dr. Daniel Timms
The first thing to point out about Daniel is that his PhD is not in medicine but in mechanical engineering. His doctoral thesis was titled “Design, development and evaluation of centrifugal ventricular assist devices.” Daniel studied mechanical engineering at Brisbane’s University of Technology.
The background development of the BiVACOR took place in Australia and the amazing story of how Daniel interfaced with the medical profession (a deeply conservative bunch and always sceptical of people outside of their profession) is told in great detail in an excellent article by [Trent Dalton and published in The Australian].
It’s a story about how some leading cardiologists recognised the potential of Daniel’s artificial heart research and threw the weight of their professional credibility behind him; it’s great stuff.
The future development of the BiVACOR initially took place in the US at BiVACOR’s Houston head office. Once again demonstrating that Australia punches above its weight when it comes to innovation but often fails to provide the financial backing to fund (and benefit from) the ultimate commercialisation.
In fact, the vital phase of funding for BiVACOR came in the form of angel investment from a Texas furniture salesman Jim “Mattress Mack” McIngvale, who gave $2.5 million.
Development of artificial hearts
Daniel’s own words from the “Abstract” of his thesis document sets the scene…
Heart disease is the developed world’s biggest killer, and the shortage of donor's hearts has accelerated the development of mechanical alternatives.
Scientists, engineers and clinicians have attempted to replicate the human heart with a mechanical device for over 50 years. Although a number of pulsating devices have been developed, and in some cases worked briefly, they have invariably failed to match the success of heart transplantation.
Building an artificial heart is no mean feat
Building an artificial heart presents a number of challenges. Firstly, blood is sensitive stuff, it doesn’t like to be thumped around by mechanical devices and damage to its components such as platelets (haemolysis) results in complications particularly blood clots (thrombosis) which can travel to other parts of the body and create life-threatening blockages (strokes).
Similarly, any rough surfaces on artificial heart devices (rough metal, imperfect joins or protruding edges) can cause localized clots that then grow in size until they shear off and travel elsewhere. Haematological compatibility is a major challenge.
Healthy real hearts are remarkable little devices with extraordinary pumping capability compared to their size and remarkable adaption mechanisms including growing bigger in response to the body’s needs.
Previous artificial hearts by comparison are big units suitable only for larger people (mostly full-grown men) ruling them out for women and children.
So, the critical problem is attempting to create a mechanical device with enough pumping grunt to fit into the same space as a real biological heart; it hasn't been done yet, efforts to date all rely on external power sources, typically a battery pack that must be worn outside of the body.
BiVACOR artificial heart - the shift from pulsatile artificial hearts to continuous blood flow
Earlier artificial hearts attempted to emulate the heart’s pulsing and were based around reciprocating pump actions requiring non-return valves; from a mechanical engineering perspective, inherently unreliable and the blood took a savage beating.
Recipients of these contraptions were chock-full of blood thinners, anticoagulants and other drugs. With artificial hearts, it’s not “if” you have a stroke but “when”.
The limitations of reciprocating pumping systems lead to the application of rotary pumps requiring shafts and bearings to locate rotating parts creating places where blood could stagnate and bearings that generated heat damaging blood proteins (protein damage starts as low as 44 degrees Celsius).
The curious topic of how the rest of the body with all its highly evolved and adapted intricate systems will react long term to a circulation system that flows continuously rather than pulses is too big to delve into here.
BiVACOR will be the first continuous flow (non-pulsatile), bi-ventricular, single unit, complete artificial heart. After a quick scan of the internet, the short answer appears to be continuous flow works fine. But, long term effects are yet to be observed. There is limited consensus about the strict requirement to deliver pulsatile perfusion to the human circulatory system.
However, should a definitive opinion emerge that a pulse is necessary BiVACOR can be modified to deliver pulsed blood flow; they are already working on it.
BiVACOR artificial heart - balancing left and right blood flow
Another remarkable property of real hearts is their ability to balance blood flow on their left and right sides. The body’s blood circulation is split into two systems;
- The pulmonary system: (blood flowing through the lungs to exchange carbon dioxide with oxygen) is pumped by the right side of the heart.
- Systemic blood flow: The left side of the heart has a much bigger pumping task because it circulates blood through the rest of the human body. However, all the blood coming out of the lungs is fed into the left side of the heart before being pumped throughout the body. Consequently, the two flows must be equal.
Failure to equalise pressure results in life-threatening complications.
For example, raised pulmonary blood pressure and the resultant increased hydrostatic pressure favours extravasation of fluid into the lung, causing pulmonary edema (fluid gathers in the lungs). In addition, sub-optimal pulmonary blood pressure has a deleterious effect on gas exchange processes. There are other adverse interactions resulting from sub-optimal pressures; in short, a balanced system is essential for maintaining health.
In a mechanical heart, equalising the flow could be achieved by having two separate pumps that are electronically controlled. This would involve embedding pressure sensors and having two drive motors. This would add size, complexity, and potentially require more power; in the interests of simplicity and therefore reliability; these are things to be avoided.
The BiVACOR artificial heart
The BiVACOR developed by Dr Daniel Timms has only one moving part – a spinning rotor fitted with impeller blades on two sides creating two pumps from one motor; one to handle the pulmonary circuit (through the lungs) the other side handles the main systemic circulation through the body.
The impellers aren’t matched incapacity; the pulmonary impeller provides roughly 10% of the pumping ability compared to another side; this is intended as flow through the pulmonary system is relatively unrestricted compared with systemic circulation (the rest of the body).
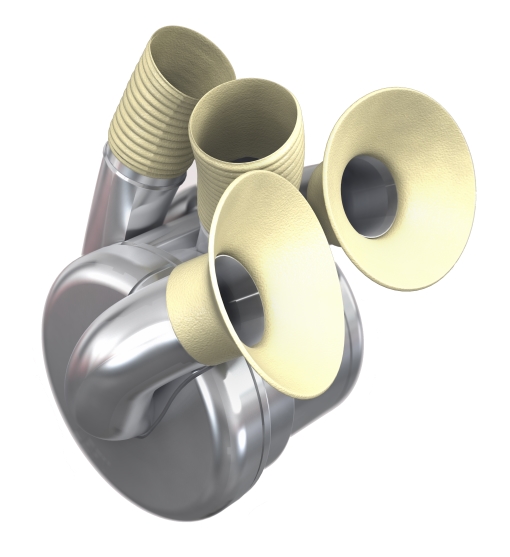
In the BiVACOR the impeller is driven by a rotating magnetic field (standard practice for synchronous electric motors) however, this same magnetic field is used to suspend the rotor in the axial direction from one side with an active magnetic coil on the other side in concert with permanent magnets.
The active magnetic coil is used for fine positioning (controlled by a microprocessor in response to three eddy-current position detectors) with the bulk of the force coming from the permanent magnets. The arrangement reduces power consumption.
The arrangement is so contrived to ensure that the impeller spins clear of the pump casing; it levitates in the axial direction and is positioned laterally pinned by magnetic fields preventing it from touching the metal sides. Clever.
Automatic blood flow balancing
But the real genius is the way in which this suspended rotor arrangement balances left and right side blood flow.
The imbalance in pressure on either side of the rotor (through natural changes in pulmonary or systemic flow resistance) causes it to displace within the confines of the magnetic field thus improving the efficiency of the impeller on the opposing side and increasing the pressure thus balancing the flow. The rotor assumes the vertical position required to maintain homeostasis. No need for two motors. It’s a self-organising system.
Simplicity is the key
Reading through Dr Timms’ doctoral thesis it is clear that considerable research and testing was undertaken to optimize the efficiency of the internal pump topography through computational fluid dynamics using media that simulated blood. This lead to the development of an optimal impeller design, pump chamber shape and inlet and outlet ports. No trivial exercise.
The result is an efficient, compact and self-flow-balancing device with one moving part and no metal to metal rubbing surfaces. A design optimized for performance reliability and long working life. The simplicity of design is paramount; compare the elegant simplicity of the BiVACOR with the French Carmat artificial heart.
Variable heart blood volume output
Real hearts vary their blood flow output in response to physiological need, primarily oxygen demand, and is controlled by the autonomic nervous system acting on the heart’s internal pacemaker the SA Node. Real hearts also modify output through changes in stroke volume varied through a process called the Frank-Starling law.
The BiVACOR varies blood volume output using pump speed which is varied by using alternating current frequency speed control in response to the body’s physiological needs (how it exactly interfaces with the body’s heart speed regulation mechanism isn’t clear to the author but I am working on finding out). The rotor speed varies somewhere from about 1,700 rpm up to about 2,500 rpm and at its maximum speed delivers 12 litres of blood per minute.
Possible future development; fully embedded operation
The device suffers one drawback being the need for the patient to wear an external power source (battery pack) and control unit. In this respect, it is no better (or worse) than previous artificial hearts. However, the BiVACOR has modest power requirements needing no more than 17 watts at full output putting it in a feasible range of being powered through a biological fuel cell.
The author speculates that one day it may be possible for the BiVACOR to be completely self-contained perhaps drawing upon the concept of using a biobattery that converts the body’s blood glucose and oxygen into electricity. Such technology is being worked on by other research teams.
Remarkably that is close to what the human heart does; converts glucose and oxygen into motive power and in a surprisingly small package.
Creating a totally self-contained (no external power pack) artificial heart would be a stunning achievement. BiVACOR puts that possibility within reach.
BiVACOR needs investment
Initial efforts to raise development capital for the BiVACOR artificial heart were difficult. However, as time has passed, funding has been found.
The BiVACOR artificial heart is an amazing first step toward realizing the objective of delivering a reliable one size fits all complete replacement for a failed heart; it’s the first artificial heart that is small enough to implant in women and children. But, later perhaps forming the centrepiece of a completely self-contained totally implanted artificial heart system (no external battery unit).
But, its not quite there yet; no doubt a few technical wrinkles to iron out, patents to pay for, animal and human trials, government approval jumps and hoops, business development, marketing tools, endless travel and accommodation. Not to mention the salaries of the dedicated team who by now ought to be earning good money (but probably aren’t) for their time invested, expertise and talent. The initial $5 million was spent fast.
Update: 17 June 2021
Total Artificial Heart to be commercialised by Monash and BiVACOR
Announced in Manufacturing Monthly, a collaboration of universities lead by Monash will work on commercialisation of BiVacor. $1 million of federal Government funding has been provided to support the venture.
Partners across Australia, Asia-Pacific, USA and Europe have been engaged and regulatory approval pathways have been established. The team has also recently closed a $19 million Series B to fund the company’s preclinical verification activities, and the addition of key team members to support the first in-human studies.
Update: 18 May 2018
Australian Venture Capital firm OneVentures backs BIVACOR
Announced in Australian Financial Review18 May 2018...
OneVentures Healthcare Fund III, established as part of the federal government's Biomedical Translation Fund initiative, has initially invested $3 million but may invest up to $10 million if BiVACOR can meet certain milestones.
This is great news. Only took 2 years, but at least now BIVACOR has significant backing. Congratulations to Daniel Timms and the team.
It seems they do have a heart.
Update: 1 October 2019
NASA Johnson Space Center to Assist BiVACOR Inc. with Artificial Heart System
Announced in Roundup Reads" NASA - Johnson Space Center
NASA’s Johnson Space Center is pairing with BiVACOR, Inc., to improve the robustness and reliability of the company’s Total Artificial Heart (TAH) system — an implantable rotary bi-ventricular blood pump and associated external electronics. On Oct. 1, the partnership was inked via a Reimbursable Space Act Agreement during a commencement ceremony.
Indeed this is great news. NASA has pioneered the development of medical technologies for human survival systems to use in their space programs. The NASA bio-science/medical team will apply their learnings and research methods to help BiVACOR to improve the robustness of their artificial heart.
Further reading
